Clinics and community health centers across the United States are rushing to adjust operations after the Trump administration implemented a rule in mid‑2025 that bans undocumented immigrants from receiving care at federally funded health centers and other federal health programs. The policy, finalized and enforced by the Department of Health and Human Services (HHS) in July, is already reshaping access to care in many communities, even as legal challenges move through the courts. As of August 18, 2025, the rule remains in effect, and clinics say patients and staff are caught between new federal limits and public health concerns.
Under the rule, federally funded health centers must not provide services to undocumented immigrants using federal dollars. The scope reaches across community health centers, HIV/AIDS programs, and other public health initiatives that, for years, treated patients regardless of immigration status. HHS has issued directives to ban undocumented patients from taxpayer‑funded programs, arguing that federal funds should not be used to serve people without legal status. Administration officials frame the change as a budget and enforcement priority, not a decision about medical need.
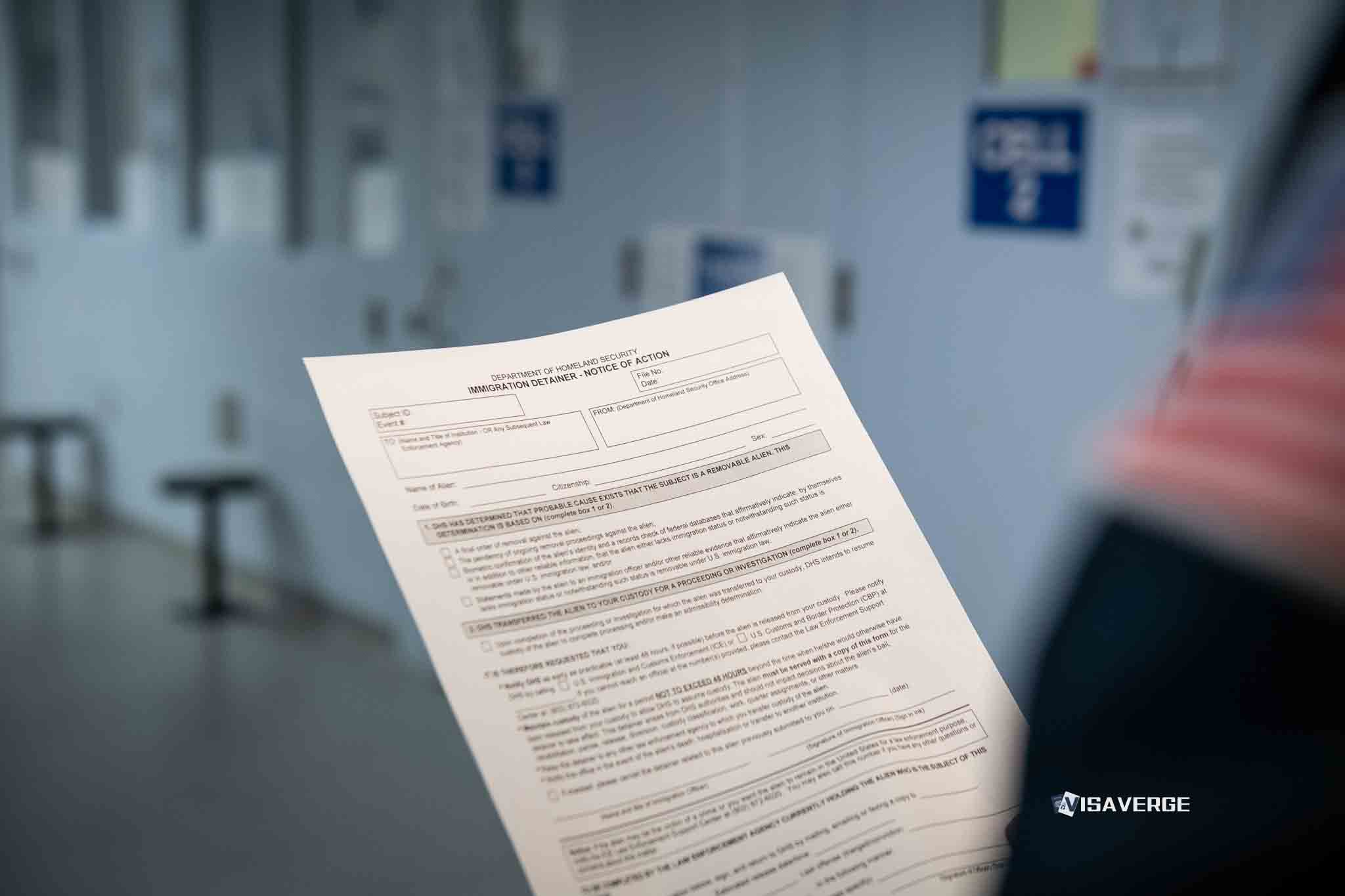
Many providers fear the policy will push people away from routine care and into emergency rooms. Clinic leaders describe scrambling to set up front‑desk screening, train staff on immigration status checks, and adjust billing systems. These steps add new administrative burdens and may trigger fear among families who worry that a visit could lead to denial of care or exposure to immigration enforcement. Public health experts warn the ripple effects will extend beyond those directly excluded, affecting mixed‑status families and entire neighborhoods.
State action and money pressures collide
Some state governments are trying to soften the blow. California, Oregon, Washington, Minnesota, and the District of Columbia continue to fund certain coverage for undocumented immigrants using state dollars. These programs aim to keep primary and preventive care available where federal funds are now off limits.
- These state programs try to preserve:
- Primary and preventive care access
- HIV prevention and treatment continuity
- Prenatal and pediatric services
Yet several efforts face stress from budget gaps and federal cuts. Minnesota, which expanded coverage to undocumented adults in January 2025, is already reconsidering parts of its program amid fiscal strain.
Money pressures intensified after President Trump signed the 2025 budget reconciliation bill on July 4, which includes more than $1 trillion in cuts to federal health program funding over the next decade. Clinic leaders say the new rule and the budget cuts together form a one‑two punch: fewer federal dollars and a smaller patient pool that is still sick but now more likely to avoid care until conditions become urgent.
According to analysis by VisaVerge.com, providers expect:
- Longer waits at emergency departments
- Higher uncompensated care totals
- Rising costs for local health systems as preventable conditions worsen
HIV prevention and treatment programs are a core worry because consistent access is vital to control transmission. In one case, a federal judge in Idaho issued a preliminary injunction that temporarily protects access to HIV medication for all immigrants, including those without legal status. While limited to specific measures, the order underscores how judges are parsing the rule and its effects program by program.
Clinics also report growing confusion about documentation. Staff must be careful when asking for proof of immigration status so they do not deter eligible patients or create discrimination risks. Many are adopting scripts that explain:
- What is required for federally funded services
- What care can still be offered through state or local funds
While the policy does not mandate sharing patient information with immigration enforcement, health workers say fear alone can keep people away—especially those who have lived through past enforcement surges.
Key takeaway: Administrative changes and fear of enforcement can lead people to avoid care, with consequences that spread beyond the individuals directly excluded.
Court fights, sanctuary stances, and what comes next
Lawsuits filed by civil rights groups, health providers, and local governments argue the rule harms public health, raises constitutional issues, and conflicts with long‑standing practice at the nation’s safety‑net facilities. For now, courts have allowed the policy to proceed while cases advance, with selective injunctions—like the Idaho order—shaping the edges.
- Courts so far have:
- Allowed the policy to remain in effect in many places
- Issued selective injunctions protecting specific services or programs
- Left open the possibility of further, program‑specific rulings
Cities and counties with sanctuary policies say they will keep their protections in place. Health agencies in those areas are exploring:
- More local funding
- Confidential care pathways
- Clear privacy rules to reassure patients
These steps cannot replace federal support, but local leaders argue they can lower the risk of outbreaks and encourage treatment for chronic diseases that, left untreated, grow more dangerous and costly.
HHS Secretary Robert F. Kennedy Jr. has said the government must stop diverting taxpayer dollars in ways that encourage unlawful entry, describing the policy as part of fiscal discipline and immigration enforcement. Immigrant advocates counter that tying clinic doors to immigration status undermines public health and ethics, noting that when people skip vaccines, prenatal care, or routine medications, the harm spreads within families and communities, not only among undocumented immigrants.
Human impact and clinic responses
On the ground, the change looks personal. Picture a father with asthma who has relied on a neighborhood health center for years. Now he must show proof of lawful status to receive subsidized care, or he has to pay full price he cannot afford. He waits until his symptoms flare, then heads to the emergency room. The visit costs far more than the inhaler that might have kept him well. School attendance drops as his child gets sick more often. The family’s stress climbs, with mental health needs rising just as counseling gets harder to reach.
Clinic managers say they are building flowcharts to separate services funded by state or local dollars from those funded federally, so they can continue some care legally. They are also:
- Training staff to point patients to non‑federal options where they exist.
- Revising consent and privacy notices to reflect new rules.
- Explaining, in plain words, why certain services are no longer available.
Families in states with no state‑funded alternatives may face the harshest choices.
Historical context and what to watch
The policy fits into a broader shift. The new rule builds on steps from the first Trump term (2017–2021) that sought to restrict access to public benefits and toughen enforcement. Earlier attempts to punish sanctuary cities met frequent court blocks. This time, the administration has paired a firm federal definition of who can be served with reduced funding, making the change harder for states and clinics to absorb.
Legal observers expect more motions seeking temporary injunctions as plaintiffs point to harms in specific programs—especially where communicable disease control is at stake. Meanwhile, state‑federal tensions are likely to escalate, with Washington warning of funding consequences while states test the limits of their own budgets and laws.
Patients and providers looking for official updates can monitor the U.S. Department of Health and Human Services at hhs.gov. HHS press contacts and agency notices about program funding and compliance are posted there.
For now, clinics are adapting day by day. They are adding immigration status checks at intake, revising consent and privacy notices, and working with local partners to build small safety nets where they can. Families are making hard decisions about when to seek care and what to risk. And courts are weighing how far a federal funding ban can reach without breaking the systems meant to keep communities healthy.
This Article in a Nutshell
A July 2025 HHS rule bans federal funding for undocumented patients at health centers, prompting states and clinics to scramble. Providers add screenings, revise privacy notices, and seek state dollars. Legal challenges and injunctions, like Idaho’s HIV medication order, create a patchwork of access and uncertainty nationwide.













